Let's Talk About Osteoporosis
We've got the doctor-approved scoop on causes, symptoms, treatments, and a jillion other facts and tips that can make life with osteoporosis easier.
byKrista Bennett DeMaio
Health Writer
Whether you’ve justbeen diagnosed or worry you could develop osteoporosis, you’re probably nervous, confused, and maybe even a little scared. That’s normal, and everyone featured on HealthCentral with a chronic condition felt just like you do now. But we—and they—are here for you. On this page alone, you’ll not only discover the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, where to find your osteoporosis community, and all the critical information to help you not just manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
Our Pro Panel
We tapped some of the best experts in the field for the most scientific and up-to-date information possible.

Stephen Honig, M.D.
Rheumatologist and Director
Osteoporosis Center at NYU Langone
New York, NY

肯德尔莫斯利,医学博士
Medical Director
Johns Hopkins Metabolic Bone & Osteoporosis Center
Baltimore, MD

Mary Jane Minkin, M.D.
Clinical Professor of Obstetrics, Gynecology, and Reproductive Services
Yale School of Medicine
New Haven, CT
骨质疏松症指很简单多孔薄nes. Your bones get so brittle, they break. As adults, we’re always losing bone mass and building new bone. Osteoporosis develops when you lose more bone than you’re creating. The underlying cause is very low bone density, and that can stem from a whole host of factors including your genetics, assigned gender and hormones, your diet, and your lifestyle choices.
The cliché “you are what you eat” applies here. Bone is mostly made of calcium, so getting adequate levels is essential. People who didn’t get enough as children—or suffered from an eating disorder such as anorexia—don’t reach their full bone mass potential, which makes them more at risk for osteoporosis later in life. To build healthy, strong bones at any age, you want to get calcium and vitamin D through foods (dairy products, fatty fishes, calcium-rich fruit and veggies) and also eat food rich in magnesium, vitamin K, and vitamin K. Avoid high-protein and high-sodium diets, as well as heavy drinking, soft drinks such as Colas, and excess caffeine, all of which can interfere with your calcium levels.
You may not be able to cure your osteoporosis, but you can stabilize your bone density levels, and even improve them a bit, preventing future fractures. If you’re prescribed drugs by your physician, take them. Beyond meds, make sure you’re getting enough calcium and vitamin D, doing weight-bearing exercise, and limiting alcohol. And if you smoke, quit.
When it comes to osteoporosis drugs, you’ve got a lot of options. The best one for you will be decided by your physician based on the condition of your bones. If you’re at high risk of fracture, you’ll likely be put on an oral drug (Fosamax or Boniva) that slows bone loss. If you’re at a very high risk of fracture, your doctor may jump to more aggressive injectable bone-building meds such as Forteo.
What Is Osteoporosis, Anyway?
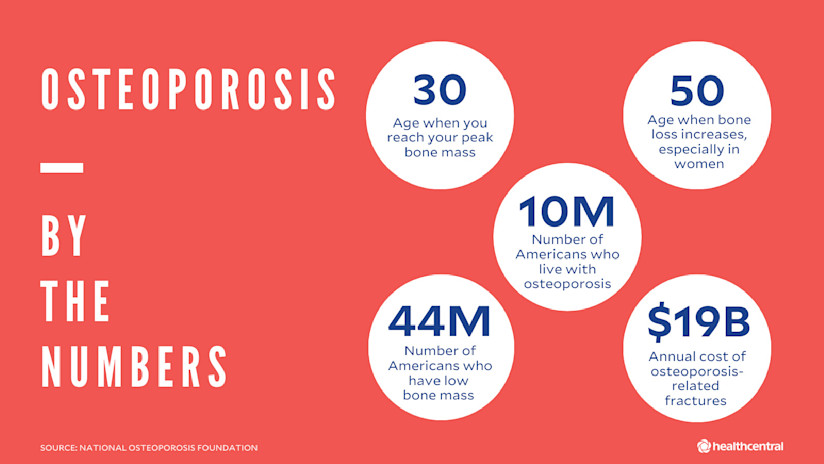
Getting a big break is generally a good thing, unless, of course, we’re talking about bones and you’re an aging adult. Then it tends to conjure thoughts ofosteoporosis. The term translates toporous, or soft, bone. Osteoporosis is a bone disease that occurs as yourbones weaken, thin, and become so fragile, they’re vulnerable tofracture(that’s the medical term for a broken bone). About 10 million Americans suffer from osteoporosis, and an astounding 44 million have low bone mass, which makes them at risk for developing the brittle bone condition, according to the National Osteoporosis Foundation (NOF).
To better understand osteoporosis, we need to talk about bone development. Here’s a crash course:
Your bones are a work in progress for most of your life, but the bulk of your bone-building happens when you’re a child and a young adult.
Bones are made ofcollagen, a protein that gives them some amount of flexibility, and alsocalcium phosphate, a mineral that gives them their strength and hardness.
The cells that build new bones are calledosteoblastsandosteocytes. Osteoclasts are cells that break down old bone and release calcium into your blood.
Around age 30, we hit what’s calledpeak bone mass—the strongest our bones are going to get. From ages 30 to around 50, your bone mass is pretty stable; you’ll lose some bone (a.k.a.resorption) and make some new bone (known asostosis), so your overall bone density remains roughly the same (a process called骨重建).
After 50, especially if you’re a woman going through menopause (more on this later), you start to lose bone more rapidly. If the bone loss outpaces the formation of new bone, you may end up withlow bone densityor even osteoporosis.
Under a microscope, the inside of healthy bone has a honeycomb-like appearance, meaning there are some small holes. But the microscopic view of an osteoporotic bone looks more like Swiss cheese; those holes are much bigger. Without medical intervention (namely osteoporosis medications), the bone loss and fragility will only get worse. Someone with severe osteoporosis can fracture a bone simply by coughing too hard or twisting the wrong way. Ouch!
What Causes Osteoporosis in the First Place?
All osteoporosis stems from low bone density, but how exactly do bones go from honeycomb-solid to weakened and resembling a wedge of Emmental? Many contributors to low bone density are beyond our control, but others are very much within it. Here’s what you can’t do much about:
Genetics:大约80%的峰值骨量是遗传的。那means the bulk of your bone make-up is determined by mom, dad, or your dear grandmother, who had osteoporosis. In addition, there are distinct hereditary conditions associated with an increased risk of osteoporosis, such as Turner syndrome and Fragile X syndrome.
Assigned gender:Women have smaller, thinner bones than men, so they tend to have a lower peak bone mass to start with. Men can get osteoporosis, too, but it’s far more common in women, especially post-menopausal white and Asian women. One in two women (versus one in four men) ages 50 and older will have an osteopathic bone break. The relationship between estrogen and osteoporosis is an important one, too. Estrogen is thought to boost those bone-building osteoblast cells. So, when estrogen plummets after menopause, bone mass tends to as well.
Age:Maintaining that peak bone mass you had at 30 is like trying to stay your wedding-day weight--never going to happen. We slowly start to lose bone mass at age 40 and more rapidly in the next decade.
Body frame:Having a petite frame can up your risk of developing the bone condition. A slight frame is associated with slight bones.
Ethnic background:Those with Northern European and Asian roots are more prone to osteoporosis. People with Mediterranean and African American backgrounds tend to have higher peak bone mass, providing extra protection against osteoporosis.
Now for those osteoporosis risk factors that youcancontrol? These include:
Weight:Being very thin is associated with a higher risk of osteoporosis, as a slender figure is associated with thinner bones. For women, weighing less than 127lbs or having a BMI less than 21 seems to increase your risk. Being overweight doesn’t help either. Obesity can lead to conditions such as diabetes, which can accelerate bone loss.
Diet:钙是年代的构建块trong bones, and vitamin D helps your body absorb the mineral. A diet that’s low in either one can result in a lower-than-normal peak bone mass. Eating a low-carb diet or one that’s high in salt can also negatively affect bone density because both ways of eating can increase the amount of calcium excreted through urine. Having an eating disorder, such as anorexia, can also rob your bones of essential nutrients. (Plus, as we’ve noted, being underweight can put you at risk.) Similarly, those who have limited their diet following weight loss surgery lack in essential nutrients and vitamins, and their bones can suffer as a result.
Smoking:Add it to the list of reasons tofinallyquit: Tobacco use has been linked to low bone density. It’s thought to affect blood circulation throughout your body, including your bones (you have blood vessels and veins within the marrow of your bones), weakening them over time.
Heavy drinking:The relationship between bone density and alcohol is hazy. Some studies have shown light-to-moderate drinking (one to two drinks a day) can boost bone density, but drinking more than two drinks a day, especially hard liquor, can reduce it by interfering with your calcium and vitamin D levels, and lowering hormone levels. And, of course, if you’re tipsy, you’re more likely to fall, which can increase your chance of fracturing.
An exercise routine (or lack thereof):Weight-bearing exercises (those that require you to work against gravity to support your body weight) help build healthy bones. Think: walking, hiking, dancing, climbing stairs and jogging, to name a few. So if you don’t move much or favor non-weight bearing activities such as swimming, you could end up with low bone density. On the flip side, extreme athletes who, say, run marathons, may have low body fat and estrogen levels, increasing their chances of developing porous bones, too.
Emotional stress:New research suggests that stress may play a role in bone health. (Is thereanythingstress doesn’t affect?) Women with high levels of stress had lower bone density six years later compared to those with lower stress levels, a study in theJournal of Epidemiology & CommunityHealth showed. Exactly how psychological stress affects bones isn’t well understood, but researchers believe stress contributes to system-wide inflammation, and inflammation can slow downosteoblasts(bone-forming cells) and promoteosteoclasts(cells that break down bone). Other studies have linked depression to lower bone density.
Medications:Many commonly used Rx drugs can lead to increased bone loss and osteoporosis. These include anticoagulants like heparin and warfarin; diuretics like furosemide (but not hydrochlorothiazide); cancer drugs like methotrexate and imatinib; seizure medications like phenobarbital, phenytoin, and carbamazepine; heartburn medications like omeprazole; antidepressant medications like amitriptyline, nortriptyline, paroxetine, and fluoxetine. If you are on any of these drugs long-term, you should discuss with your physician about your risk of osteoporosis and the need for alternative medications, if necessary.
Chronic diseases:Several chronic illnesses also accelerate bone loss and up your odds of developing osteoporosis. These include hyperparathyroidism, celiac disease, and rheumatoid arthritis. If you have any of these conditions, your treatment regimen should be established to address the risk of osteoporosis from these diseases.
Will I Experience Symptoms of Osteoporosis?
Probably not. Osteoporosis is often a silent disease. In fact, most people don’t know they have it until—bam!—they break a bone. Fractures in specific areas—your spine, hip, humerus, rib, pelvis, or wrist—that occur without a large amount of trauma is a red flag for your doctor. One of the most common breaks that people with osteoporosis tend to get is aspinal compression fracture(a.k.a. collapsed vertebrae). If you have osteoporosis, you can get one of these fractures without even falling; sometimes by simply twisting the wrong way. In that case, you may notice pain in your back.
Also, there’s a reason you may picture a hunched-over old lady at the mere mention of osteoporosis. Shrinking significantly in height or developing poor posture are both signs of the condition. It’s normal to lose half an inch per decade after age 40, but more than that could be due to osteoporosis.
How Do Doctors Diagnose Osteoporosis?
So if osteoporosis is usually silent, how does it manage to get noticed? It’s typically found two ways: most often, after afragility fracture(a break that results from a low amount of trauma), or during a routinebone density scan.
Fragility Fractures
If you’ve just fractured a bone that’s vulnerable to osteoporosis (hip, spine, humerus, rib, pelvis, and wrist), and have some of the risk factors (say, you’re a post-menopausal woman or have a family history of porous bones), your doctor doesn’t even have to check your bone density to know that you have the condition. The fracture alone is enough to confer the diagnosis.
Bone Density Scan
Still, your physician will likely send you for a bone density scan, a test that measures yourbone mineral density (BMD). The most common BMD test is adual-energy X-ray absorptiometryorbone densitometry, referred to as a DXA or DEXA scan. It uses a low level of radiation to measure even small amounts of bone loss. It’s typically done on the lower spine and hips on an outpatient basis at a radiology facility or medical office, and takes less than 30 minutes. Wear comfy clothes without zippers, and let your technician know if there’s any chance you could be pregnant. You’ll also need to avoid calcium supplements for 24 hours prior to the test.
Your BMD results come in the form of a numerical score called aT-score, a measure of how your bones stack up to a 30-year-old adult of the same gender. Now, if you’re 75 years old, that hardly seems fair, right? So, why age 30? That’s when we typically hit peak bone mass, so the test shows just how far (or little) your bone mass has strayed since then. How to read your T-score?
-1 and higher is considered normal—you’ve got healthy bones
-1.1 to -2.4 is consideredosteopenia, low bone density that’s not osteoporosis
-2.5 and below qualifies as osteoporosis—soft, fragile bones that are at risk of fracture
The T-score helps your doctor decide the best osteoporosis treatment for you.
If you haven’t fractured anything, you may get your diagnosis though a routine bone density scan. When can you expect one? The U.S. Preventive Services Task Force (USPSTF) recommends that post-menopausal women receive their first scan at age 65; at risk women can start before this age. However, many gynecologists prefer to do a baseline scan within a few years of menopause. The USPSTF doesn’t have a recommendation for men, but other organizations, including the National Osteoporosis Foundation, suggest screening men at 70 years old.
The FRAX Test
Your physician may also recommend aFRAX test, which uses your bone density and other risk factors to determine how likely you are to fracture a major bone (hip, spine, forearm, or shoulder) within the next 10 years. Your FRAX score can also help determine your course of treatment.
Which type of doctor should you see if you’re concerned about osteoporosis? No one specialist is completely dedicated to the condition. Low bone density and osteoporosis can be diagnosed and treated by:
Endocrinologists
Gynecologists
Rheumatologists
Physiatrists (physicians who focus on physical medicine and rehabilitation)
.中国ists
Geriatric medicine doctors
Osteopenia vs Osteoporosis: What’s The Difference?
Osteoporosis is one of several skeletal systems diseases that can cause bone loss. There’s alsoosteopenia, which, as we mentioned above, is low bone density that has not quite reached the level of osteoporosis yet.
If you have osteopenia, you’re still at risk of fracture compared to someone with normal bone density, only less so than someone with osteoporosis. Experts say a diagnosis of osteopenia is often a wake-up call to their patients to take better care of their bones through diet and exercise, and to stop bone-destructive behaviors such as smoking. Osteopenia is typically not treated through medication.
Your doctor may also use a bone density scan to diagnoseosteomalacia(a softening of the bones typically caused by vitamin D deficiency and digestive and kidney disorders) andPaget’s disease of the bone(a bone remodeling disorder that can be crippling).

What Is The Best Treatment For Osteoporosis?
There areseveral widely prescribed osteoporosis medications, and while they may work differently, the overall goal is the same: prevent fractures. Not everyone with an osteoporosis diagnosis goes home with a script, at least not at first. If a woman in her 50s is diagnosed through a routine bone density scan, she’s active, healthy, and her FRAX score indicates that she’s at a low risk of fracture, she may not receive any treatment at all. For those with a higher risk of fractures, meds will probably be part of the picture.
Medications for Osteoporosis: You’ve Got Options
To manage your osteoporosis and prevent it from worsening, your treatment plan may include one of the following types of drugs. (And take note: It's important to adequately replete calcium and vitamin D levels before embarking on drug therapy.)
Antiresorptives
This category of osteoporosis drugs works by slowing down bone loss, giving your natural bone production a chance to catch up. Several types of FDA-approved antiresorptives agents are on the market today, including:
Bisphosphonates:这是首选的一线药物osteoporosis. Oral bisphosphonates include Boniva (ibandronate), Fosamax and Binosto (alendronate), Actonel and Atelvia (riesdronate). They’re given daily, weekly, or monthly depending on the type. Reclast (zolderonic acid) is a bisphosphonate given via intravenous infusion once a year.
Possible side effects:
Nausea
Heartburn
Esophageal irritation
Gastric ulcers
Bone, joint, or muscle pain
The IV fusions can cause flu-like symptoms that stop within a few days after your treatment. You may have heard about a scary side effect calledosteonecrosis of the jaw(loss of blood supply to the jaw bone) but experts say this is extremely rare, and usually occurs in people on high doses for cancer or after having oral surgery.
Another less common side effect is a fracture (ironic, right?), but not the type associated with osteoporosis. These meds can cause fractures in the upper thigh calledatypical femoral fractures.
Also, people with advanced chronic kidney disease should exercise caution when taking these medications as there is a heightened chance of more side effects and complications.
RANKL inhibitor:Prolia (denosumab) is an injection given every six months. However, there is some recent data about increased risk of vertebral fracture after the discontinuation of denosumab, so the need for indefinite treatment needs to be discussed with people before this medication is started.
Estrogen:Hormone replacement therapy (HRT) taken orally or via transdermal patch can help slow bone loss after menopause. Estrogen as an osteoporosis treatment is controversial because it’s been linked to health concerns, including breast cancer. Gynecologists will only consider it for patients dealing with severe menopausal symptoms (hot flashes, vaginal dryness, etc.)andlow bone density.
Selective Estrogen Receptor Modulators (SERMs):Evita (raloxifene), for instance, is an oral hormone-like medication that’s taken daily. Side effects of SERMs can include hot flashes, increased risk of blot clots, and temporary flu-like symptoms.
Tissue Specific Estrogen Complex (TSEC):Duavee (bazedoxifene) combines estrogen with an estrogen antagonist to treat menopause symptoms. It’s shown to increase bone mineral density in the hip and lumbar spine.
Anabolic Agents
These drugs help build up your bones, so they’re less likely to break. Their function is to activateosteoblasts, those cells responsible for new bone formation. They’re considered more aggressive in preventing fractures than antiresorptives, so are typically reserved for more severe cases—those at the highest risk of fracture.
Anabolic agents are limited to one or two years use (depending on the drug) due to potentially serious side effects. The drug romosozumab-aqqg increases your risk of heart attack and stroke, while teriparatide and abaloparatide have been shown in animal studies to cause osteosarcoma, a rare bone tumor, with long-term use.
Afterwards, an anti-resorptive is prescribed to maintain new bone growth. In some cases, an anabolic is prescribed in addition to a bisphosphonate: Combining the bisphosphonate zoledronic acid with the anabolic teriparatide boosted the bone mineral density in the spine and hip more than either drug alone, according to a study in theJournal of Bone and Mineral Research.
Anabolic agents are all administered through injections, including:
Evenity(romosozumab-aqqg), given once a month for up to a year
Forteo(teriparatide) andTymlos(abaloparatide), taken daily for up to two years
Possible side effects:
Headaches
Nausea
Fatigue
Joint pain
If a fear of side effects is keeping you off meds, know this: The benefits of fracture prevention (and associated complications) far outweigh the risks of taking osteoporosis medications, according to new treatment guidelines for postmenopausal women from the Endocrine Society published inThe Journal of Endocrinology & Metabolism.
The guidelines state that women with a high risk of fractures should be treated, but then reassessed with a bone density scan after three to five years. If they’re no longer at risk, they can take a break from treatment. Women who are still at high risk should remain on the drugs. Your physician will track changes in your bone density (not less than every two years).
Other Types of Osteoporosis Treatments That Can Help
Osteoporosis is a chronic condition, absolutely, but there are a host of things you can do—in addition to typical meds—to help you feel your best. You may want to try the tactics that follow, with the help of specialists like a trainer or nutritionist.
Fall prevention:A physical therapist or personal trainer can help you boost core strength, which is huge for improving balance. To reduce your chances of falling and suffering a break, you’ll want to:
Wear low-heeled shoes with rubber soles,
Remove area rugs that may slip under your feet
Always hold a rail when going downstairs
Weight-bearing exercises:This doesn’t necessarily mean heavy weight-lifting; it’s any exercise that requires you to support your weight: walking, dancing, hiking, yoga, yardwork. Resistance training with weights or bands can also build bone mass (muscles, too). If you’re at high risk of fracture, you’ll want to avoid jarring, high-impact workouts such as running, but these low-impact exercises are very much recommended.
Diet:Getting morecalcium—1200 mg a day for women and 1,000 mg for men--is key for bone building. Milk, yogurt, cheese, broccoli and sardines are all great sources. If you’re not big on dairy, a calcium supplement can fill in the gap.Vitamin Dhelps your body absorb calcium, and you can get it through sunlight and foods such as vitamin-D fortified milk and fatty fish. If your vitamin D levels are low (your doctor can check with a blood test), take a supplement. Beyond those vitamins, eating aMediterranean-based diet(lean meats, veggies, fruit, nuts, and olive oil) may reduce hip bone loss in one year, according to research from the University of East Angila.
Smoking Cessation:This is one thing that cannot be stressed enough. Smoking cigarettes accelerates bone loss. Any treatment regimen for osteoporosis is incomplete if it does not incorporate strategies for smoking cessation. If you need help to stub out your habit, visit the American Heart Association for supportquitting smoking.
To ease the pain associated with osteoporotic fractures, your doctor may recommend OTC medications including acetaminophen or ibuprofen. You might also want to explore these drug-free treatments:
Acupuncture
Biofeedback
Massage
Transcutaneous electric nerve stimulation, which reduces pain via electrical impulses
Is Osteoporosis Reversible?
To some extent, it can be. Your bones aren’t inert: There’s alwayssomeremodeling taking place within them. So, with the right treatment, exercise, and a good diet, you may actually improve your bone density. But doctors say stability—not losing any more bone mass, rather than building more of it— is what defines success with this condition.
Can You Prevent Osteoporosis in the First Place?
Yes, osteoporosis is preventable, to some extent. Remember, the bulk of your peak bone mass is inherited, but you still have control over many bone-building factors (like those below) that determine how strong and resilient your bones will be.
Think of your bones like a retirement account. If you start saving money early, planning for the days when you’ll no longer work, you’ll be ahead of the game when you need the money. Likewise, if you focus on building healthy bones before you start losing bone mass, you’ll have more “bone” in the bank when your body starts making withdrawals. But it’s never too late to start saving. If your BMD scan shows osteopenia, focus on these good bone habits:
Eat a bone-healthy diet, which means:
Calcium-rich foods(dairy products, sardines and salmon with bones)
Fruits and veggiesrich in calcium, magnesium, vitamin C and vitamin K (leafy greens, broccoli, red peppers, oranges) and fortified foods like cereals and bread
Limiting foods and beverages that can interfere with calcium absorptionsuch as high sodium foods, excessive amounts of protein, caffeine and colas
Taking a calcium and/or vitamin D supplementif needed
Do weight-bearing exercise for at least 30 minutes on most days
Quit smoking
Limit alcohol
Get enough sleep: Women who slept less than five hours a night had lower bone density than those who got the suggested seven hours of shut eye, a study in theJournal of Bone and Mineral Researchfound.
What’s Life Like for People Living with Osteoporosis?
If you’ve been diagnosed with osteoporosis in your 50s, and you make those important lifestyle changes to boost your bone health, chances are, your quality of life won’t be greatly affected. But people with more severe cases of osteoporosis who have had multiple fractures can suffer serious complications. Is osteoporosis painful? It can be. Plus, hip and spine fractures can lead to a loss of mobility, not to mention a loss of independence as well as financial stress due to healthcare bills.
You may also feel scared about falling or breaking bones, which can lead to anxiety and social isolation. Some people experience depression after repeated fractures, especially those that limit mobility. This can all cause a downward spiral, considering that anxiety and depression have also been shown to lower bone density. Having a support system, whether that’s a mental-health professional or an online community of people who share your struggles, may help alleviate some of your stress and concerns.

So, Where Can I Find My Osteoporosis Community?
Osteoporosis is largely an invisible disease. Unless you have X-ray vision, you’ll never know who else is walking around with porous bones. Finding others in your shoes may take a bit more digging than it does for other conditions. Fortunately, we did the sleuthing for you. Jump in and share your pain and success stories, gain resources and education, and, hopefully, draw some strength (literally and figuratively) from these resources.
Top Osteoporosis Non-Profits and Support Groups
National Osteoporosis Foundation. This isthe领导组织骨质疏松和头脑lth. While you’re there checking out tips, statistics, treatment options, and the latest research, drop into their online community viaInspire.comwith message board topics including bone-healthy recipes, exercise and physical therapy, support for men with osteoporosis or osteopenia, and pain relief.
American Bone Health. No bones about it, medical lingo can be confusing. This site translates the topic of bone density into easy-to-understand terms. There’s even a hotline you can call with specific questions. Take a quiz to see how vulnerable to fracture you are. Then pop into the online community to gain tips and support from people in the same boat.
Save Our Bones. If you’re looking for holistic ways to strengthen your bones, the Save Institute’s Save Our Bones program can get you started. Here, you’ll get access to a free at-home kit, articles, and products that take a natural approach to bone density.
Top Bone Health-related Bloggers
苏珊布朗博士,博士,更好的骨头,betterbones.com
They should call Dr. Brown “Dr. Bones,” because she focuses her life’s work on bettering your body by bettering your bones. As a medical anthropologist and a certified nutritionist, Dr. Brown prides herself on using only natural methods to help you build strong bones. Check out her science-backed six-point program that has helped tens of thousands of women rebuild their bone strength. Here, you can expect easy strength-training routines, nutrition tips, and the latest in bone research.
Dr. Lani Simpson, D.C., Bone Health Blog,lanisimpson.com
As a chiropractor and certified densitometrist (that’s “bone doctor” for those who don’t know), Dr. Simpson saw a need for integrated and holistic practices to come together to deliver patients the best of all medicine worlds. She brings research-backed info to her blog to help you choose the methods that are right for you.
Dr. Sophie Toland, Osteopathy, Anatomy and Yoga,sophietolandyoga.com
After suffering many injuries in her teen years, Dr. Toland took to osteopathy—an alternative treatment that manipulates muscle tissue and bones—to rebuild her strength. She saw what it did to not only rebuild, but make her bones stronger, and she began helping others. Now, she combines her love of osteopathy, anatomy, and yoga—which, let’s face it, are all intertwined—into online courses to help others.
Top Osteoporosis-Related Podcasts
Bone Talk. Created by the National Osteoporosis Foundation, this podcast/blog combo delves into conversations about managing your pain, building healthy bones, and the latest research.
Bone Banter. As you’ve guessed, this science-y podcast covers international news and research related to bone health.
- Osteoporosis Facts and Figures:National Osteoporosis Foundation. (n.d.). “Osteoporosis Fast Facts.”cdn.nof.org/wp-content/uploads/2015/12/Osteoporosis-Fast-Facts.pdf
- Women, Weight, and Osteoporosis:Journal of Bone and Joint Surgery. (2003). “Older Women With Fractures: Patients Falling Through the Cracks of Guideline-Recommended Osteoporosis Screening and Treatment.”insights.ovid.com/bone-joint-surgery-american-volume/jbjs/2003/12/000/older-women-fractures-patients-falling-cracks/5/00004623
- Bone Density and Alcohol:American Journal of Clinical Nutrition. (2009). “The Effects of Beer, Wine, and Liquor on Bone Mineral Density in Older Men and Women.”ncbi.nlm.nih.gov/pubmed/19244365
- Stress and Low Bone Density:Journal of Epidemiology & Community Health. (2019). “Psychosocial Stress and Bone Lose Among Postmenopausal Women: Results from Women’s Health Initiative.”jech.bmj.com/content/73/9/888
- Depression and Bone Density:Brain and Behavior. (2016). “Bone Density and Depressive Disorder: A Meta-Analysis.”ncbi.nlm.nih.gov/pmc/articles/PMC4980464/
- Anabolic Agents for Osteoporosis:Journal of the Endocrine Society. (2018). “Osteoanabolic Agents for Osteoporosis.”ncbi.nlm.nih.gov / pmc /文章/ PMC6065487 /
- Osteoporosis Drug Treatment Guidelines:The Journal of Clinical Endocrinology & Metabolism. (2019). “Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice Guideline.”academic.oup.com/jcem/article/104/5/1595/5418884
- Combining Drug Treatments:Journal of Bone and Mineral Research.(2011). “Effects of Intravenous Zoledronic Acid Plus Subcutaneous Teriparatide in Postmenopausal Osteoporosis.”ncbi.nlm.nih.gov/pubmed/20814967
- Hip Fracture Mortality Rate:World Journal of Orthopedics. (2019). “Changing Trends in the Mortality Rate at 1-Year Post Hip Fracture.”wjgnet.com/2218-5836/full/v10/i3/166.htm
- Emotional Health and Osteoporosis:Frontiers in Psychiatry. (2019). “Impacts of Psychological Stress on Osteoporosis: Clinical Implications and Treatment Interactions.”ncbi.nlm.nih.gov/pmc/articles/PMC6465575/